A do-not-resuscitate (DNR) order form is an order written by a physician to withhold lifesaving measures if a patient goes into cardiac or respiratory arrest. Unless a patient has a DNR order on file, healthcare personnel will begin cardiopulmonary resuscitation (CPR) when necessary.
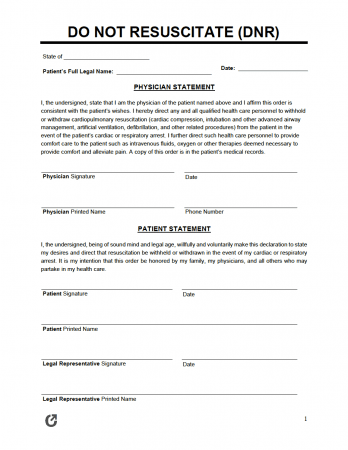
The principal, or the individual completing the document, must be mentally sound and coherent when filling out the DNR form. If the principal becomes incapacitated (i.e., they cannot make decisions for themselves), an appointed agent can create the document in their place.
Each state has specific rules and regulations for DNR forms, such as statutes for signing, witnesses, and notarization. The principal must reference local laws to ensure they have satisfied the state’s requirements.
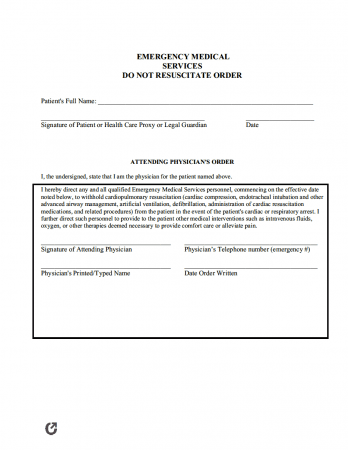
“Do-not-resuscitate” means that a patient does not want medical personnel to save their life if they experience cardiac or respiratory arrest. If a patient completes a DNR form, healthcare professionals and emergency medical technicians (EMTs) cannot legally revive them. Lifesaving procedures include chest compressions, electric shocks from a defibrillator, intubation, or medication.
Physicians, nurses, and other medical staff can attempt to resuscitate an unresponsive patient if they have not completed a DNR form. For example, if the patient is in “full code,” their heart has stopped beating, or they are no longer breathing. In this case, the healthcare team would give the patient CPR, blood transfusions, intravenous fluids, electric shock, medication, or other treatment to bring them back to life.
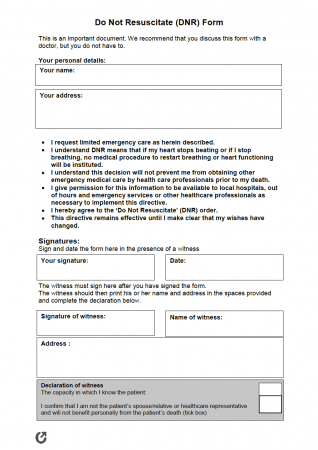
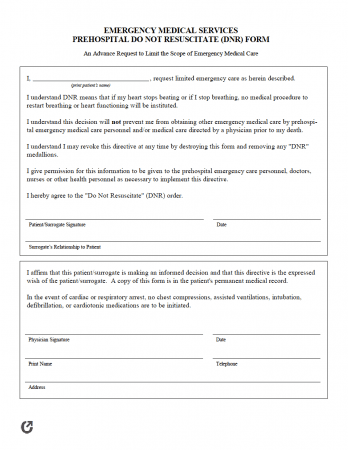
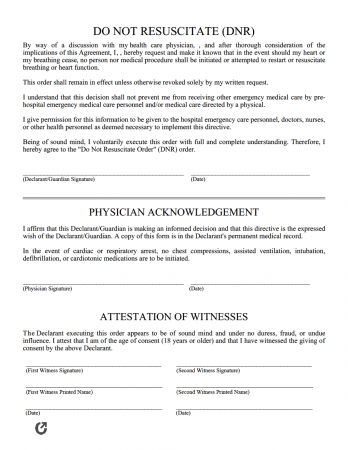
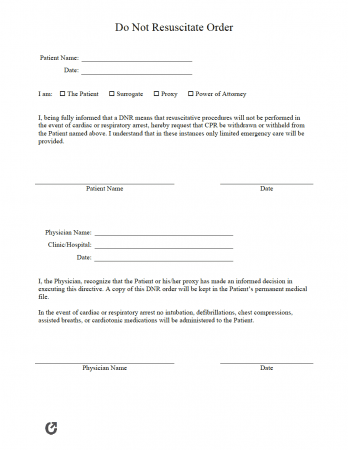
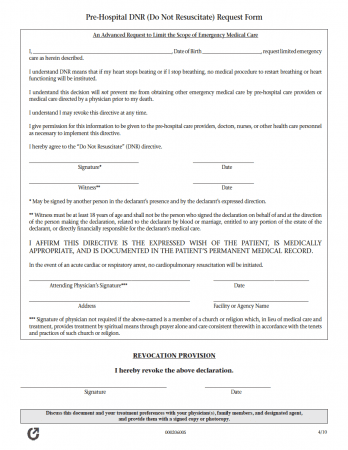
Individuals can create a do-not-resuscitate order in several ways: 1) by signing a specific hospital’s DNR form in the presence of a physician, 2) writing a formal letter, or 3) using a template. Regardless of the method, individuals generally begin the process by taking the following steps.
Before completing the DNR form, the individual must make an appointment with their primary care physician to discuss their wishes. Patients who temporarily reside in the hospital must discuss the matter with the doctor overseeing their care.
Due to the seriousness of the DNR order, the patient must put their wishes into writing. The physician must sign or acknowledge the form to validate it. Medical staff cannot honor a verbal do-not-resuscitate order as it does not prove the patient’s consent. The physician (or other medical professional) becomes liable for the patient’s death if they do not perform lifesaving measures without an official DNR.
Once the principal creates the document and discusses it with their doctor, they must file it with the hospital or office. Adding it to the patient’s medical chart informs all healthcare personnel of their DNR wishes.
The principal should have a conversation with their loved ones about their medical preferences. Family members or friends may or may not agree with the decision to deny lifesaving measures. However, the individual should inform their relatives, either way, to help them understand why the medical staff cannot perform the life-sustaining treatment.
A principal can appoint a family member or friend as their agent by completing a medical power of attorney. The court assigns an agent for incapacitated patients who do not have a signed power of attorney. Once granted authority, the agent can make medical decisions for the principal.
The assigned person must feel confident while carrying out the patient’s wishes. For example, the agent must consider whether they feel comfortable authorizing the patient’s DNR order. Similarly, they must agree to make DNR decisions for the patient if they have not expressed their medical preferences in writing.
Laws for do-not-resuscitate orders vary according to each state’s jurisdiction. For example, Illinois mandates that the principal, physician, and one (1) witness over eighteen (18) sign the form. However, Maryland instructs only the physician to sign.
Other states have laws that only apply to their residents. Florida, for instance, requires that the principal completes the form on yellow paper. The state does not accept the form if the individual uses any other paper color.
By creating a DNR order, the patient denies life-sustaining treatment. In contrast, individuals use an advance directive to outline their medical wishes if they become incapacitated. By completing a DNR, the individual refuses electric shock, CPR, medication, breathing machines, or other life-sustaining care. However, an advance directive informs the appointed agent of the preferred treatment, such as artificial and hydration, if they become incapacitated.
More specifically, an advance directive is a comprehensive document that combines a medical power of attorney and a living will. The medical power of attorney form allows the assigned agent to make decisions for the principal without their approval. However, when acting as the agent, they must make choices based on what they feel the principal would want in the specific situation. The second part of the form, otherwise known as the living will, allows the document’s creator to express their desires for medical intervention and end-of-life care. Unlike a DNR form, the principal uses a living will to include preferences for pain management, organ donation, mechanical ventilation, and other health-related treatment.
As with DNR state laws, each state has rules for advance directives. Depending on where the individual lives, the advance directive may need witnesses to sign, or it may need to be notarized. Consulting state law resources or a trusted lawyer can ensure individuals have reliable and valid information.
A do-not-resuscitate form allows the medical staff to deny a patient’s lifesaving treatment. The document states that the principal wishes to naturally die if they suffer from a condition that causes their heart to stop beating or their lungs to stop breathing.
Before filing the DNR order, the principal must ensure that the form adheres to state laws. Otherwise, medical professionals have no choice but to perform CPR, intubate, or give medication that helps to bring the patient back to life. Once the patient officializes the document, they must submit it to their doctor’s office, hospital, skilled nursing facility, or hospice care. At that time, the office staff adds it to the individual’s medical record for future use.
Although not required, the principal can combine an advance directive with a do-not-resuscitate form. Combining both legal documents gives the medical professional team confidence in carrying out the patient’s wishes as requested. Without a DNR form or advance directive, the appointed agent must determine the best course of treatment. The agent must make rational decisions while experiencing high amounts of stress, such as that experienced during the death or medical emergency of a loved one. However, making sensible choices at this time can prove challenging. Therefore, having a form that clearly states the patient’s desires can help direct the agent and medical staff’s course of action.
Nobody can override a patient’s DNR order. Medical professionals must follow the requests written in the form, even if their judgment opposes it. Family members, spouses, and close friends cannot revoke a DNR order either.
Patients write do-not-resuscitate orders to express their end-of-life preferences. Individuals can create the form at any stage in their life; however, people who prepare their advance directive most commonly complete this document along with it. Furthermore, those who have experienced previous medical challenges or received a terminal illness diagnosis may use a DNR form to convey their wishes if they become unable.
Similarly, individuals with a high risk of illness, injury, or death can fill out the document to deny medical treatment. For instance, if the person suffers from a heart attack, stroke, or another similar medical event, they can choose to pass away rather than receive care.
Elderly, chronically ill, or terminally diseased patients might deny medical resuscitation as it can cause them more pain or suffering. Similarly, those who suffer from physical injuries might not wish to receive treatment. For example, the physical pressure from CPR might break the person’s ribs or further complicate their injury or illness.
The patient must discuss their DNR wishes with their physician upon admittance to a hospital, skilled nursing facility, or hospice. The physician must ensure that the patient understands a DNR order and its outcomes. A patient can weigh its pros and cons to decide whether the choice is right for them.
The list below contains the state laws for DNR orders. States that do not have statutes use the abbreviation “N/A.”
The patient and physician are required to sign in most states. However, Georgia, Iowa, Maryland, Ohio, and Oregon only require a signature from the physician. Kentucky is the only state that does not order a physician to sign. Notarization is not required; however, a form that includes a Notary Public seal or stamp holds more authenticity. Therefore, the patient should have the document notarized, if possible.
| STATE | WITNESS OR NOTARY? | STATUTE |
| Alabama | Not required. | § 420-5-19-.02 |
| Alaska | Not required. | AS 13.52.150 |
| Arizona | Yes; One (1) Witness. | § 36-3251 |
| Arkansas | Not required. | § 20-13-904 |
| California | Not required. | PROB § 4780(3)(c) |
| Colorado | Not required. | § 15-18.6-102 |
| Connecticut | Not required. | § 19a-580d |
| Delaware | Not required. | § 2509A |
| Florida | Not required. | FAC 64J-2.018 |
| Georgia | Not required. | § 31-39-(2-9) |
| Hawaii | Not required. | § 327K-2 |
| Idaho | Not required. | § 39-4514 |
| Illinois | Yes; One (1) Witness. | 755 ILCS 40/65 |
| Indiana | Yes; Two (2) Witnesses. | § 16-36-5 |
| Iowa | Not required. | § 144A.7A |
| Kansas | Yes; One (1) Witness. | § 65-4943 |
| Kentucky | Yes; Two (2) Witnesses OR Notary Public. | § 311.623 |
| Louisiana | Not required. | § 40:1155.3 |
| Maine | Not required. | § 93-A.1(b) |
| Maryland | Not required. | § 5-608 |
| Massachusetts | Not required. | None. |
| Michigan | Yes; Two (2) Witnesses. | § 333.1053 |
| Minnesota | Not required. | Chapter 145C |
| Mississippi | Not required. | § 41-41-302 |
| Missouri | Not required. | § 190.603 |
| Montana | Not required. | § 37:10 |
| Nebraska | Yes; DNR – One (1) Witness for DNR; Declaration – Two (2) Witnesses OR Notary Public. | § 20-404 |
| Nevada | Not required. | § 450B.520 |
| New Hampshire | Not required. | § 137-J:26 |
| New Jersey | Not required. | N.J.A.C. 10:48B |
| New Mexico | Not required. | § 7.27.6.8 |
| New York | Not required. | Senate Bill S7883 |
| North Carolina | No, UNLESS a Declaration (Two (2) Witnesses AND Notary Public). | § 90-321; § 90-322 |
| North Dakota | Not required. | § 23-06.5 |
| Ohio | Not required. | § 3701-62 |
| Oklahoma | Yes; Two (2) Witnesses. | § 63-3131.5 |
| Oregon | Not required. | § 847-035-0030; § 847-010-0110 |
| Pennsylvania | Not required. | § 5481 – § 5488 |
| Rhode Island | Not required. | R23-4.11-MOLST |
| South Carolina | Not required. | § 44-78-10 – § 44-78-65 |
| South Dakota | Not required. | ARSD 44:05:06; SDCL 34-12F |
| Tennessee | Not required. | § 68-11-224 |
| Texas | Yes; Two (2) Witnesses OR a Second Physician. | § 157.25; Chapter 166 |
| Utah | No, UNLESS Patient is a Minor (Second Physician). | R432-31 |
| Vermont | Not required. | § 9708; § 9709 |
| Virginia | Not required. | § 54.1-2987.1 |
| Washington | Not required. | § 43.70.480; § 70.245 |
| West Virginia | Not required. | § 16-30C |
| Wisconsin | Not required. | § 154.17 – § 154.29 |
| Wyoming | Not required. | § 35-22-501 – § 35-22-509 |
Individuals have a right to direct their medical care, even if they cannot communicate it. A do-not-resuscitate form orders physicians, emergency medical technicians, and other medical personnel to honor an individual’s request not to receive CPR if it becomes necessary.
Ideally, DNRs are set in place before they become necessary; however, medical events can leave a person unconscious or unable to communicate their wishes. Sometimes family members of an unconscious individual are left wondering what choice to make if their loved one’s heart or breathing stops. Establishing an advance directive, including the DNR form, can help clarify a person’s wishes and ensure they receive the interventions – or not – they desire.